ERISAExpress Wrap Documents
Wrap documents using OCA’s ERISAExpress™ platform, including both the required SPD and Plan document, are fully compliant and take minutes to create. The system also stores documents for seven years making it easy to find and manage current and past documents.
Fully-Customized
Competitive Pricing
Guaranteed Compliance
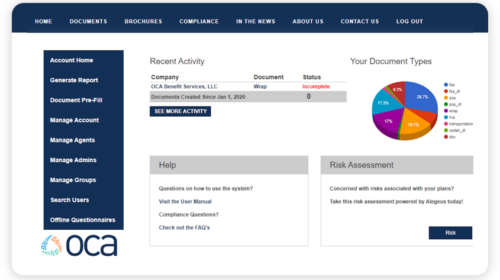
Wrap Documents Made Easy!
The Employee Retirement Income Security Act of 1974 (ERISA) requires group health plans to have a written plan document and a summary plan description (SPD). The SPD needs to be provided to all participants upon enrollment in the plan. Insurance carrier documents including the contract, policy or certificate booklet (collectively, the certificates) do not generally satisfy the ERISA requirement. Why don’t they? – Insurance companies are not required to create an ERISA-compliant SPD. While many carriers will provide Certificates and plan information, these typically do not contain the required language or provisions to satisfy ERISA. This can open the employer up to liability and fines.
Why Wrap Benefits?

Use One Document
Use one document to satisfy the ERISA SPD requirement and other disclosure requirements.

File one Form 5500
File one Form 5500 rather than a separate one for each benefit.

Stay Compliant
Failure to meet ERISA’s requirements can result in significant penalties imposed by the DOL.
Guaranteed Compliance
OCA’s team works with a nationally recognized law firm to have all questions, help tools, and documents reviewed. There is no need for you to watch for regulatory updates regarding your documents; OCA and its compliance team will monitor updates for you!
High Level Overview of Potential Penalties
Failure to meet ERISA’s requirements can result in significant penalties imposed by the DOL:
- Up to $110/day, per plan
- Failure-to-file penalties of up to $1,000 per day, per plan
- IRS penalties of $25 per day up to $15,000 per year, per plan
- Individual penalties for other breaches of fiduciary responsibilities
Wrap Document FAQs
Wrap Requirements
If an employer is subject to ERISA they’re required to:
Have a written plan document for each group and welfare benefit plan
Have a SPD for each group and welfare benefit plan
Keep their plan records for 6 years
File an IRS Form 5500 if they have more than 100 participants
Provide all of the ERISA required language
ERISA Required Language
A majority of carriers do not provide all of the above information in their benefit booklets or certificates.
Plan Name
Plan Number
Plan Year
Employer’s Tax ID
Name and Address for Plan’s legal agent
Named Fiduciaries
Procedures for amending/terminating the plan
Eligibility terms
Source of Plan contributions
Info on the responsibilities for the operation of the plan by ER, Carrier and TPA
Defined claims procedures
Subrogation Info (statement identifying situations that may result in loss or denial of benefits)
ERISA statement of participant’s rights
Plans Subject to ERISA
Fully insured group health plans (subject to ERISA and state insurance laws)
Self-funded group health plans (subject only to ERISA)
Dental plans
Vision plans
Group term life insurance plans
Accidental death and dismemberment insurance
Insured disability benefits
Prescription drug plans
Health flexible spending accounts
Medical expense reimbursement plans
Health reimbursement arrangements
Executive medical reimbursement plans
EAP plans
Wellness plans
Onsite clinic arrangements that are integrated with an employer’s group health plan
Schedule a Demo with OCA
OCA’s ERISAExpress service can help deliver the experience and business results you’re looking for.
Request a Demo