COBRA Toolkit 101
Access our COBRA toolkit guides below, which will help ensure you’re fully aware of all the COBRA obligations, procedures, and timelines throughout the year.
Clients must communicate with OCA when one of the following actions occur.
Scenario 1
General Rights Notice for New Enrollees
Explained Further: The initial notice obligation could arise when, for example- employees or their spouses or dependents who have previously declined coverage enroll at open enrollment; a covered employee gets married and his or her new spouse becomes covered by the plan; or a newly hired employee and his or her spouse become covered by the plan following any eligibility waiting period.
Employer Action: The initial notice must be issued to the covered employee (and spouse, if applicable) within 90 days after coverage begins. Click here to watch a video tutorial on how to submit an Initial Right Notice request to OCA.
Scenario 2
A COBRA Qualifying Event Occurs
Explained Further: COBRA has a list of seven specific triggering events. Those events include termination of a covered employee’s employment (other than for gross misconduct); a reduction of a covered employee’s hours of employment; the death of a covered employee; a divorce or legal separation from the covered employee; ceasing to be a dependent child under the terms of the plan; the covered employee’s becoming entitled to Medicare; and employer bankruptcy (this relates only to retiree plans).
Employer Action: When a COBRA event occurs, as the employer you have a maximum of 30 days to notify OCA of the event. OCA will then send out an Election Notice to the qualified beneficiaries (QB) last known address. The QB will then have 60 days to make an election. Click here to watch a video tutorial on how to submit a COBRA qualifying event request to OCA.
Scenario 3
Employer Updates Benefit Plans/Rates
Explained Further: If/when rates are updated or new benefit plans are added, please remember to communicate those changes to OCA! This ensures the information provided by OCA to newly qualified beneficiaries (QBs) and existing COBRA participants is accurate and timely.
Employer Action: Employers will need to notify OCA if/when they update their benefit plan/rates throughout the year. Simply click the link below to complete our “COBRA Renewal Form.”
COBRA Quick Guides
Employer COBRA Portal Guide/Overview
Our COBRA solution is a first-of-its-kind cloud-based offering. It enables highly efficient COBRA administration for employers of all sizes and complexity and delivers unrivaled flexibility in scale, configurable reporting, and a highly intuitive user experience.
The Lifecycle of a COBRA Participant Guide
This guide is meant to be a general overview of the lifecycle of qualified beneficiary and COBRA participant. We discuss the roles and responsibilities of the employer, OCA, and participant and what actions need to be taken when a COBRA qualifying event occurs, participants terminate COBRA, how COBRA disbursements work, etc.
COBRA Letters Flow Chart
Ensuring the delivery and confirmation of a COBRA letter is critically important. This guide will explain all the trigger rules in place that would prompt OCA to issue a COBRA letter to any participant.
The Lifecycle of a COBRA Participant

Step 1 – Suspend Coverage with Carrier(s)
The employer will need to suspend/terminate the qualified beneficiary’s coverage(s) with the insurance carrier(s) per the terms of the employers SPD(s).

Step 2 – Communicate Qualifying Event to OCA
When a COBRA event occurs, as the employer you have a maximum of 30 days to notify OCA of the event. We have attached an instructional guide on how to submit a qualifying event through OCA’s secure employer/broker portal.

Step 3 – Election Notice is Mailed
OCA must notify the qualified beneficiary generally within 14 days after receiving a qualifying event notice. Providing the election notice is the most critical step in COBRA administration. Generally, the qualified beneficiary’s election period will not end until at least 60 days after OCA provides the election notice is mailed.

Step 4 -Qualified Beneficiary Elects & Pays COBRA
COBRA coverage is not automatic. A qualified beneficiary must affirmatively elect-within the election period to continue his or her group health plan coverage. If elected, OCA will send specific email communications to the necessary eligibility contacts. The email will come from noreply.oca@wealthcarecobra.com.

Step 5- Reinstate COBRA Participant in Elected Plans
OCA will email the employer eligibility contacts when a new participant elects coverage and fully pays their initial premium. The eligibility contact (typically the employer) is then responsible for reinstating coverage with the specified carrier(s).

Step 6- Collecting & Disbursing COBRA Premium
OCA will issue premium disbursement twice (2) per month to the employer. Disbursements will be made to the employer via ACH or paper check. OCA charges $2 per check disbursement. ACH is included at no charge. Employers will have access to payment & disbursement reports through OCA’s COBRA employer portal.
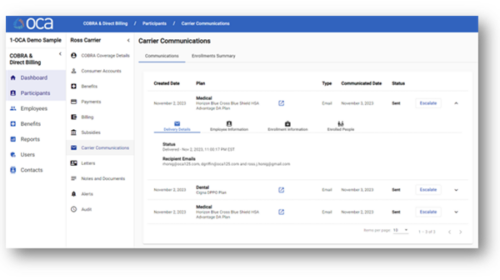
Client/Carrier Contact(s) Enrollment Communication Options
OCA will send system-generated emails to inform designated client contacts, which may include Employers, Carriers, and Brokers, about the enrollment status of COBRA participants. Clients are responsible for specifying the contact(s) for their organization during OCA’s COBRA onboarding and renewal paperwork, with the flexibility to modify contacts throughout the year. Although OCA can relay COBRA enrollment notifications, it is important to note that OCA does not provide audit support post-communication. This means OCA does not verify the reinstatement of a COBRA participant or address inquiries related to the client’s monthly insurance invoice. Additionally, OCA will not access a client’s HRIS/Payroll system or a carrier system to input data. Clients are advised to consult with their carrier or broker for details on communicating with carriers about coverage changes and COBRA eligibility/exhaustion, as carriers may require direct data entry by employers into their
COBRA Portal Video Tutortials
Adding a New Hire
Describes how to submit a New Hire/New Employee to OCA using OCA’s COBRA Employer Portal.
Submit a Qualifying Event
Describes how to submit a Qualifying Event to OCA using OCA’s COBRA Employer Portal.
How to run a Disbursement Details Report
Describes how to create a Disbursement Details Report. This report allows clients to identify the details associated with disbursed premium.
Schedule Employer Training
OCA is happy to provide training on our employer portal. Our employer portal will allow you to submit enrollments/terminations, retrieve COBRA notices, identify your COBRA participants and more! To schedule training with OCA, please click the button below.
Schedule COBRA Training